Minimally invasive sterilization for canines and felines
Laparoscopic procedures help minimize tissue trauma and allow same-day discharge.
For many veterinarians, spays and neuters are the first surgeries that they learn and can be the most frequently performed throughout their careers. Even though this is considered a routine procedure, surgical technique has continued to evolve. Minimally invasive surgery (MIS) has transformed how we approach both complex and straightforward cases in veterinary medicine.
Laparoscopy has become a viable and increasingly accessible option for elective sterilization in canines and felines. As equipment becomes more affordable and training is more widespread, veterinarians can see firsthand how laparoscopic techniques can benefit patients, clients, and practices.
The core principles of MIS are to achieve the same surgical goals while minimizing tissue trauma. For laparoscopic sterilization procedures, this means using 1 to 3 small incisions to gain access to the abdomen via laparoscopic ports, insufflating with CO2 for visualization and working space, and using specialized instruments to seal and transect ovarian, uterine, and testicular structures.
Compared with traditional open approaches, laparoscopic surgery results in less postoperative pain, smaller incisions, faster recovery, and improved cosmetic outcomes. Patients typically require less analgesia postoperatively and can return to normal activity within days rather than weeks. For the surgeon, laparoscopic surgery allows for excellent visualization because of enhanced magnification and illumination. This is particularly advantageous when working in small or less accessible regions of the body, such as the caudal abdomen. For owners who are increasingly attuned to comfort, cosmesis, and recovery, these benefits are compelling.
Laparoscopic ovariectomy
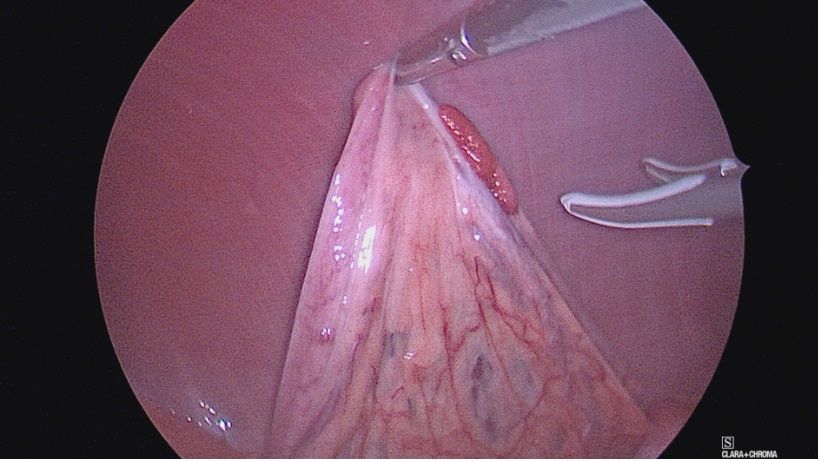
Laparoscopic ovariectomy is a procedure in which the ovaries are removed via 1 to 3 small incisions, often with the aid of a vessel-sealing device. After insufflation, the ovaries are identified and suspended, either with graspers or a transcutaneous suture, and the ovarian pedicles are then either sealed or ligated with suture and subsequently removed from the abdomen (Figure 1).
Several studies have shown a reduction in postoperative pain scores compared with traditional open ovariectomy or ovariohysterectomy. Because removal of the uterus is not necessary in most young and healthy patients, ovariectomy achieves sterilization while minimizing anesthesia time and tissue trauma.
Laparoscopic ovariohysterectomy
Although laparoscopic ovariectomy is the most commonly performed minimally invasive sterilization, ovariohysterectomy is also feasible and can confer some of the same benefits to the patient with regard to reduced pain and a faster recovery. Laparoscopic ovariohysterectomy can be performed for cases in which uterine pathology is suspected and is appropriate for some patients with pyometra (Figure 2). This approach has been reported to be feasible, associated with a low risk of conversion, and requires less rescue analgesia in patients undergoing laparoscopic ovariohysterectomy compared with a traditional open approach.
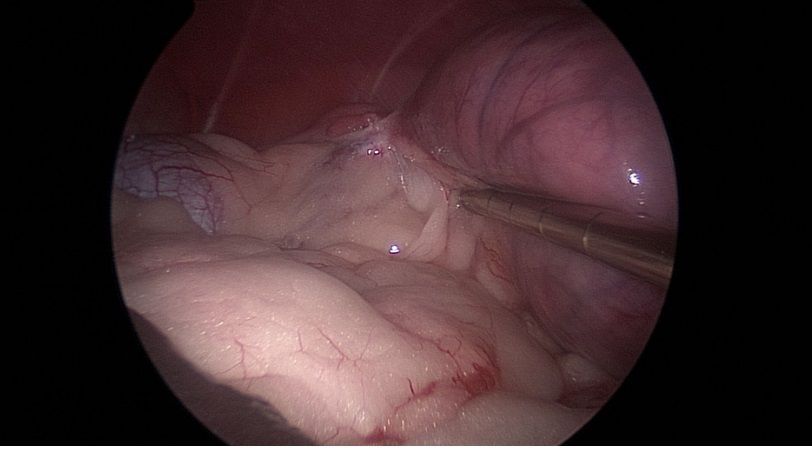
Similar to a laparoscopic ovariectomy, this may be performed with 1 to 3 ports, depending on the surgeon's preference. The surgeon begins by grasping and retracting the ovaries and sealing or ligating the ovarian pedicle. Following this, the broad ligament is continually broken down with the aid of a vessel-sealing device bilaterally until the remainder of the uterus can be gently exteriorized. The ports are removed, the incision is lengthened to facilitate placement of a wound retractor, and the remainder of the ovariohysterectomy is performed extracorporeally.
Laparoscopic cryptorchidectomy
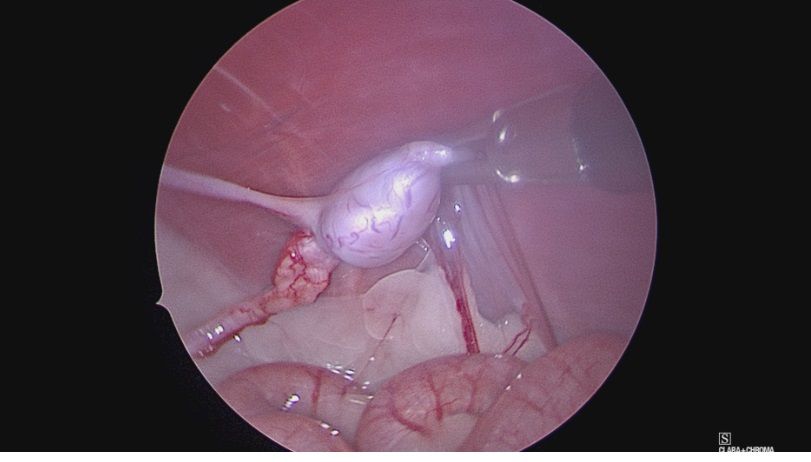
Laparoscopy allows for excellent visualization and access to abdominal cryptorchid testicles in comparison with open approaches (Figure 3). Furthermore, open approaches may be challenging or limited, and have been reported to be associated with iatrogenic injury to the prostate, bladder, and ureters. The testes are able to be identified easily in the caudal abdomen and can be grasped directly to allow exposure to the ductus deferens and testicular vessels. These vessels are sealed and transected in a similar fashion to a laparoscopic ovariectomy and removed from the abdomen.
Don’t forget about the cats!
Although most of the early literature focused on dogs, laparoscopic sterilization is also feasible and has similar advantages in cats. Feline laparoscopic ovariectomy can be performed using 3- to 5-mm instruments in a similar fashion to dogs. Laparoscopic sterilization in cats allows the same benefits as it does in dogs, resulting in less pain, a smaller and more cosmetic incision, and a faster recovery.
Laparoscopic cryptorchidectomy is also feasible in feline patients and allows for excellent visualization of the retained testicle. Although working space can be challenging, this can be improved by the use of smaller instruments and percutaneous sutures for retraction.
Postoperative management
Patients that undergo laparoscopic sterilization are generally able to be treated as an outpatient and can be discharged the same day. Postoperative analgesia may include opioid medications while in the hospital, and most patients will benefit from the administration of an oral nonsteroidal anti-inflammatory drug upon discharge. Patients should be exercise-restricted for 10 to 14 days postoperatively and encouraged to wear an Elizabethan collar, or potentially a surgical suit in the case of feline patients. The risk of complications following laparoscopic sterilization is low, but does include hemorrhage, infection, and dehiscence.
